How to Treat Patellofemoral Pain
- Category: Knee, Sports Medicine, Blog
- Posted On:
- Written By: Myra Trivellas, MD
This is part two of common injuries in female athletes and how to treat them.
How to Treat Patellofemoral Pain
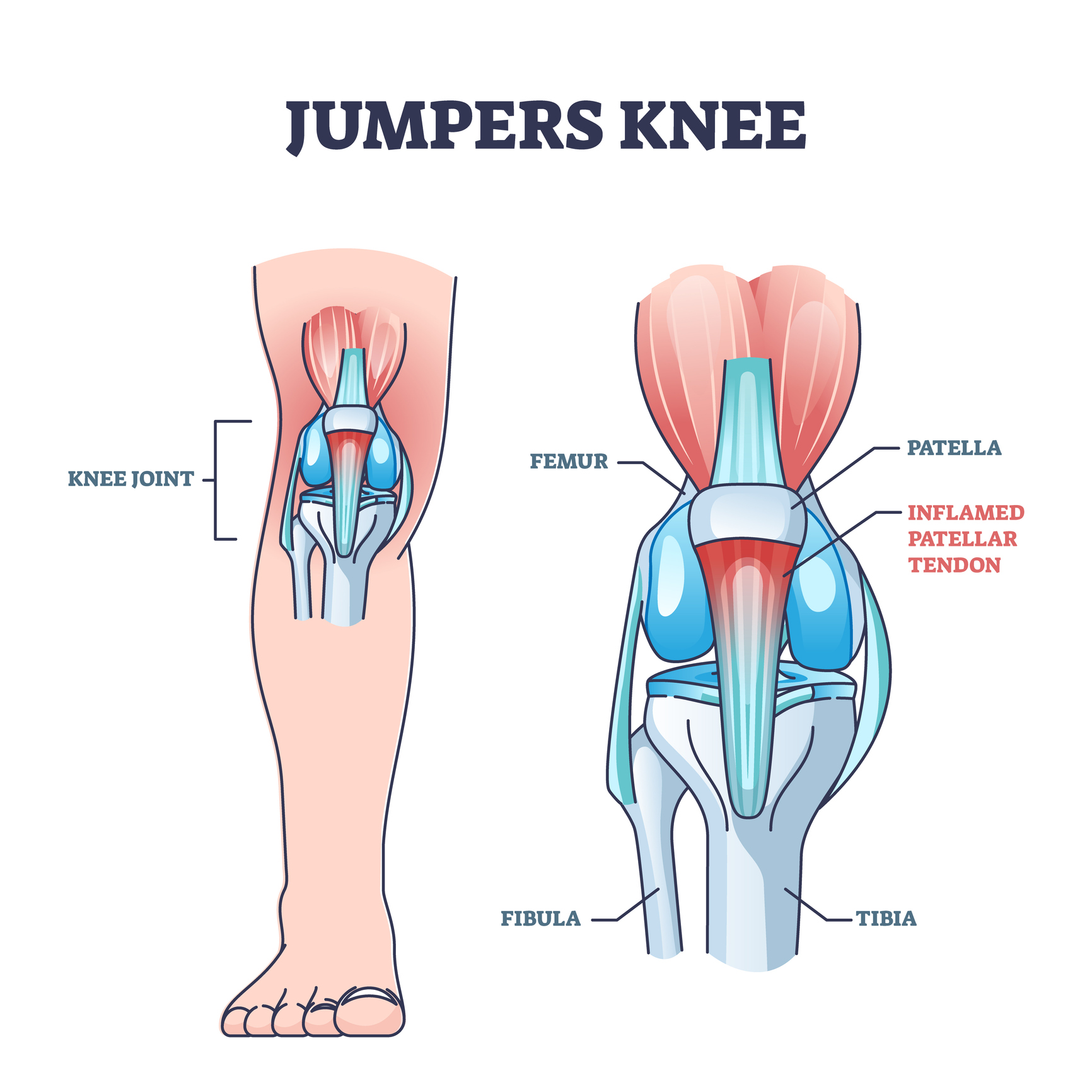
The knee is made up of three bones; the femur, the tibia and the patella. The patella sits within the quadriceps muscle and connects the femur to the tibia through the patellar tendon. This area, also called patellofemoral, is a common spot for injuries in both male and female athletes.
Women will have an increased risk of patellofemoral symptoms, as females have wider hips and different lower extremity alignment than men. Furthermore, they tend to be more flexible than men, which can lead to injuries from their ligaments being too loose.
What types of patellar injuries are most common?
 Injuries to the kneecap can occur in a spectrum of severity and can be a one-time dislocation of the patella (knee cap) or recurrent instability events. A dislocation of the patella is caused by a direct impact or a misstep that forces the patella out of its normal grove. The patella can sometimes relocate on its own or may provide further care from a medical professional. It is common for the patella to dislocate again if it has already occurred. If there is a structural component to the athlete’s anatomy that makes them more prone to their knee cap dislocating, surgery may be helpful to re-align their knee and prevent future dislocations.
Injuries to the kneecap can occur in a spectrum of severity and can be a one-time dislocation of the patella (knee cap) or recurrent instability events. A dislocation of the patella is caused by a direct impact or a misstep that forces the patella out of its normal grove. The patella can sometimes relocate on its own or may provide further care from a medical professional. It is common for the patella to dislocate again if it has already occurred. If there is a structural component to the athlete’s anatomy that makes them more prone to their knee cap dislocating, surgery may be helpful to re-align their knee and prevent future dislocations.
Overuse injuries can also occur from repetitive impact common in jumping and running, causing inflammation of the patella tendon, otherwise known as Jumper’s Knee. The athlete will have pain at the bottom of the patella and will occur most often when bending the knee. Physical therapy is the first step to strengthen the muscles around the knee, especially the quadriceps, which provides critical stability to the knee. Stretches are also very helpful to balance the athlete’s leg and decrease pain and stiffness. Strengthening core muscle groups such as hip abductors, core/abdominal muscles, quadriceps (specifically the inner quad, VMO), and muscles supporting the knee will improve the athlete’s overall stability and significantly protect against injuries. Flexibility in your hips and lower back is also important.
In addition to strengthening and stretching to prevent injury further, what are other ways to treat Patellar injuries?
For a short time after injury, activity modification to allow for rest and recovery may be necessary. The goal afterwards is to build back in a balanced way to return strong and healthy.
Seeing a primary care physician with a specialty in sports medicine is a good idea if an injury does not improve within 1-2 weeks with standard treatment such as R.I.C.E.
If the athlete has pain with weight bearing or if there is swelling in their joints that does not resolve in 5 days, they should see their doctor and have imaging ordered.
Athletic trainers or physical therapists can be incredibly helpful in guiding athletes when to see an orthopedic surgeon. For non-operative care such as concussion monitoring or ankle sprain management, a primary care physician or an athletic trainer can provide guidance and monitor for safe return to sports.
About the author: Myra Trivellas, MD is an orthopedic sports medicine surgeon with Hoag Orthopedic Institute. She played Division 1 lacrosse during her undergraduate education and continued her involvement in sports throughout medical school and residency. Her education, experience and research on female athletes and injuries gives her an in-depth perspective on how to treat sports injuries that we are excited to share with you.