Pain Management
↑The following section shares details about how to help you manage pain, before and after your surgery. Pain affects everyone differently and with the guidance of your doctor and care team, the following tools can assist you with managing your pain.
Choose a Section Below
Understanding Pain
Pain is not just physical—it’s shaped by how your brain interprets signals from your nerves. That’s why people can experience pain differently, even after the same procedure. Pain can be sharp and quick, or last a long time. Your brain tells you where the pain is and how bad it is, helping you react and take care of your body.
How Can You Tell If Someone Is in Pain?
When someone is hurting, their body might show signs like:
- Tight muscles
- Breathing fast or shallow
- A fast heartbeat
- Grimacing
If you notice these signs, you can try calming your body with relaxing activities like deep breathing or mind-body activities to help with stress and feelings. This can help you feel better when you're stressed or in pain. Doing this often can teach your body to stay calm and hurt less over time.
What to Know About Pain After Surgery
After orthopedic surgery, some pain is expected—it’s your body’s way of healing. It’s normal for your pain levels to go up and down. This is expected and usually improves with time and proper care.
You might feel more pain if:
- You just finished therapy
- You forgot to apply ice to the sore area
- You didn’t keep the surgical site elevated
- You’ve started taking less pain medication

Strategies for Feeling Better with Less Pain
Start Early: It’s best to begin treating pain right away so it doesn’t get worse or last a long time.
Different Medicines: Your healthcare provider will use a combination of medicines to help in different ways—this is called a multimodal approach to pain management.
Personal Plan: Everyone is different, so healthcare providers make a special plan just for each person.
Comfort Measures: To support healing and pain management, use these comfort measures to help you explore various ways you can manage your pain:
- Rest
- Ice
- Elevation
- Relaxing music
- Pray/meditate
- Reposition
- Breathing exercises
- Walk
What is Multimodal Pain Management?
Multimodal pain management involves using a combination of medications and techniques—like acetaminophen, NSAIDs, nerve blocks, and relaxation strategies—to target pain from multiple angles. This approach can improve comfort, reduce the need for opioids, and support a smoother recovery. It’s all about helping you get Back to You.
Why use a Multimodal Approach?
- Improves overall pain relief and comfort
- Reduces opioid requirements and related risks
- Supports a speedy recovery and progression in therapy
- Lowers incidence of surgical complications linked to poor pain control
It's common for people to worry about taking pain medication after surgery due to concerns about side effects or addiction. However, avoiding pain medication entirely may lead to increased discomfort and slower recovery. Research shows that patients who use pain medication appropriately to manage post-surgical pain often end up needing less medication overall than those who delay or avoid it.
Below is a list of medications that may be part of your multimodal pain management plan. Not all will apply to you—your provider will help decide which are appropriate based on your needs and recovery goals. CAUTION: Take any medications only as directed by your physician.
Purpose, Potential Side Effects & Precautions
| Medication / Treatment | Details |
|---|---|
| Acetaminophen |
|
| NSAIDs |
|
| Muscle Relaxants |
|
| Medications for Neuropathic Pain |
|
| Opioids |
|
| Nerve Blocks |
|
When to Call Your Provider
- Pain remains greater than 6/10 despite following the plan
- Signs of medication reaction: rash, difficulty breathing, severe nausea
- New symptoms: swelling, redness at surgical site, fever greater than 102°F
- Confusion or extreme drowsiness

Important Reminder: Pain is a highly individual experience, and what works for one person may not work for another. This multimodal approach is intended as a flexible guide. Always communicate openly with your care team about your pain levels and any side effects so your plan can be personalized to your needs.
How Does Cold Therapy Help?
Cold therapy, also called cryotherapy, can effectively reduce pain and inflammation. By applying cold to the affected area, it numbs the pain, reduces swelling, and decreases muscle spasms. Here are some of the benefits of cold therapy and practical tips on how to use it for pain relief.
Cool the Pain-Calm the Mind
After surgery, cold therapy can help your body feel better with less pain.
It works in two main ways:
- Cold therapy cools the skin and slows down the pain signals traveling to your brain. This numbing effect helps reduce how much pain you feel.
- Cold therapy also slows blood flow, which helps bring down swelling and inflammation. It can relax sore muscles and may even reduce the need for pain medication.
Altogether, using cold therapy can make recovery more comfortable and support healing.
Cold Therapy Tips
- Use gel ice packs most of the day as needed
- Always apply with a barrier (towel/single layer of clothing) to protect the skin
- Best for acute pain, post-surgical recovery, joint swelling
How Can Deep Breathing Help Pain?
Deep breathing is a simple yet powerful technique that can help reduce pain by promoting relaxation and reducing stress. By focusing on slow, deep breaths, you can activate the body's natural relaxation response, which can decrease muscle tension and lower the perception of pain. Here are the benefits of deep breathing and practical tips on how to incorporate it into your pain management routine.
Benefits of deep breathing techniques
- Your body has a system that helps it rest and heal. Deep breathing turns this system on, so you feel less pain and calmer.
- Deep breathing helps slow your heart rate and lower your blood pressure, which allows your body to relax.
- It also loosens tight muscles that might otherwise restrict blood flow.
- When you're feeling anxious, taking slow, deep breaths can calm your body and help you feel more grounded and in control.
Deep breathing helps reduce stress hormones and provides more oxygen to the brain, which can ease anxiety—especially the kind that comes with both short-term and long-term pain. It signals to the body that there’s no need to stay “on alert”, helping shift you into a calmer, more peaceful state.
Deep Breathing Techniques
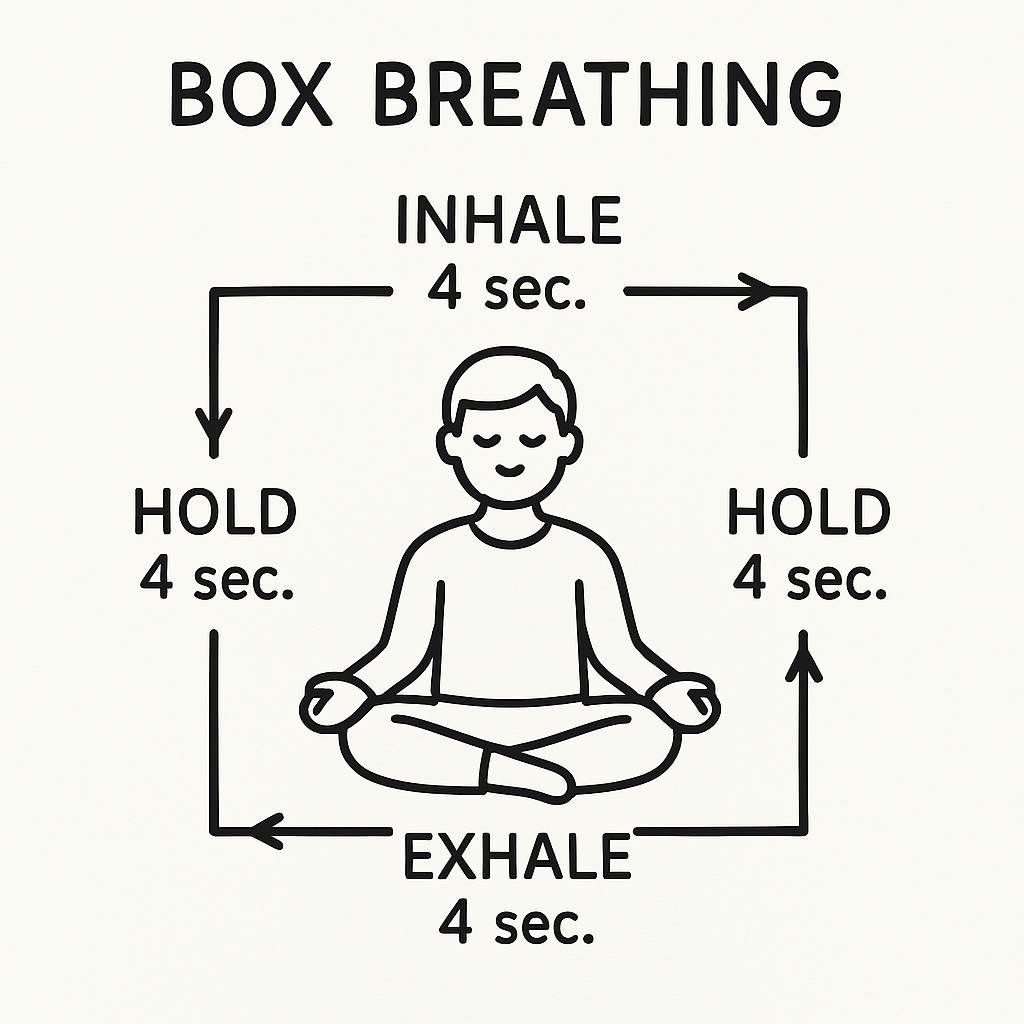
Box breathing:
- Breathe in slowly for 4 seconds
- Hold your breath for 4 seconds
- Breathe out slowly for 4 seconds
- Hold your breath for 4 seconds
Diaphragmatic Breathing:
- Breath from the belly, not the chest
- Use during pain flares or before therapy sessions
How Does Sleep Help Improve Pain?
Quality sleep helps the body repair and regenerate, reduces inflammation, and improves overall pain tolerance. It’s important to understand the connection between sleep and pain relief. Here are some practical tips for improving sleep quality to better manage pain.
Benefits of Sleep
Improves Physical Well-Being: Sleep supports healing and helps maintain a healthy weight, making it essential for surgical recovery.
Improves Mental Health: Sleep reduces stress and boosts attention and memory—key for recovery and well-being.
Improves Emotional Stability: Sleep helps stabilize mood, supporting emotional balance during recovery.
Lack of sleep may cause:
- Fatigue
- Difficulty concentrating
- Mood changes
- Irritability
- Memory problems
How does Sleep Help Impact Your Recovery?
- Sleep helps your body heal
- Helps to improve pain
- Boosts the immune system
Screens and Sleep: Impacts of Nighttime Use
Using electronic devices before bed is a common habit, with more than half of Americans regularly engaging with screens in the hour before sleep. However, this behavior can interfere with the body’s natural sleep-wake cycle. The light emitted from screens—especially blue light—can delay the body’s transition to sleep by affecting the natural signals that help us wind down at night. This disruption can make it harder to fall asleep and reduce overall sleep quality.
Tips for Healthy Sleep Habits
- Create a regular sleep schedule
- Get at least 7 hours of sleep
- Allow time to wind down
- Avoid alcohol and excessive caffeine prior to bedtime
- Stay active and head outdoors each day if possible
- Make your sleep space a sanctuary
- Reserve your bed for sleep
- Establish a "digital curfew"
- Use blue-light filters or night modes on screens
- Choose to view calming activities on electronic devices instead of stimulation content
NOTE: Sleep disturbance is reported by many patients after surgery for days to weeks. Try the tips above to minimize disrupted sleep. If you are resting or napping during the daytime hours, you may have a lower sleep requirement at night.
How Can Nutrition and Hydration Help Pain?
Eating healthy foods and hydration are vital for overall health and can help your body feel better and hurt less. Consuming optimal nutrition, anti-inflammatory foods, and staying adequately hydrated can help calm down pain/swelling (inflammation)in your body. Here are some essential nutrition recommendations and practical tips.
Benefits of diet and nutrition
People with chronic pain often have higher levels of inflammation in their bodies, which can worsen their symptoms. Whole foods contain natural compounds that help reduce this inflammation, making diet and nutrition an important part of managing chronic pain. Certain nutrients can ease pain by fighting oxidative stress—an imbalance between harmful free radicals and protective antioxidants. On the other hand, unhealthy eating habits can contribute to the development and worsening of chronic pain. That’s why an anti-inflammatory diet can be a valuable addition to other treatments in a team-based approach to pain management.

Dietitian Suggestions
Aim to include a Mediterranean Style Diet. Follow primarily plant-based eating pattern or Mediterranean eating pattern that includes high consumption of fruits, vegetables, legumes, whole grains, dairy, olive oil, moderate consumption of fish, and small amounts of red meat.
| Food Group/Nutrient | Recommendation | Why | Practical Tips |
|---|---|---|---|
| Fruit and vegetables | Aim for variety and wide range of bright colors. Think about the colors of the rainbow. | Phytonutrients are natural parts of plants that help the body fight swelling and cell damage. | Nutrients are retained through freezing. Use frozen fruits and vegetables to increase variety and reduce food waste. |
| Breads, Cereals, and Grains | Select wholegrain and fiber-rich options. | Fiber and prebiotics improve gut health and feed the gut microbiome that can play a role in pain and inflammation. | Select whole grain options when choosing bread, pasta, and rice. |
| Meat and meat alternatives | Focus on oily fish, legumes, nuts, and seeds. Can select lean meats such as chicken, fish, and small amount of red meat. | Contain healthy fats which reduce inflammation. Beans and Lentils are plant proteins that help your body stay strong. | Replace processed meats with lean meats. Choose tinned fish and legumes to save time with meal prep. |
| Dairy and dairy alternatives | Choose high quality dairy foods (milk, cheese, and yogurt). | Contain proteins to build strength, variety of fats, and important vitamins and minerals for joint health. | Use reduced fat options. Pre-sliced or grated cheese reduces prep time. Individual yogurt containers make easy snacks. |
| Healthy Fats and Oils | Include Omega-3 and monounsaturated fats. | Reduces inflammation. | Swap cooking oil for extra virgin olive oil. Include nuts and seeds such as chia, flax, and walnuts. |
| Herbs and Spices | Include turmeric, ginger, and cinnamon. | Helps your body fight swelling. | Add them in cooking, smoothies, and juices. |
| Drinks | Consume 2-3 liters water per day. Limit caffeine. | Dehydration increases sensitivity to pain. | Carry a water bottle and set a goal to finish it daily. |
| Added sugar and ultra-processed food | Reduce cakes, cookies, candy, soda, and processed meats like bacon. | Excess sugar and processed foods can worsen inflammation and damage cells. | Choose minimally processed foods at home instead of convenience foods. |
Do you enjoy lattes?
The Warm Golden Latte is a favorite to help keep you on track daily with a healthy diet for your bones. The bonus is you get to select your milk of choice and enjoy the other health benefits from spices.
- 1 cup milk or unsweetened dairy alternative milk.
- ½ teaspoon turmeric powder
- 1/8 teaspoon ground ginger
- 1 pinch ground cinnamon
- 1 pinch ground black pepper, 1 teaspoon maple syrup or honey
- In a small saucepan, whisk together the milk or dairy alternative and the dry ingredients and place over medium heat until the mixture begins to bubble. Stir in the maple syrup or honey and enjoy a warm latte.
How Does Mindfulness Help Pain?
Mindfulness means paying close attention to what is happening right now. It helps people become more aware of their thoughts, feelings, and body. After surgery, people often need different strategies to manage pain—and mindfulness can be one of them. Laughing and positive thinking are also important tools that can help with pain and overall healing.
Laughter
Laughter offers a surprising number of health benefits that go beyond just lifting your mood. It helps your heart, lungs, and muscles work more efficiently by increasing oxygen intake and stimulating circulation. Laughing also triggers the release of endorphins—your brain’s natural “feel-good” chemicals—which can help reduce the perception of pain. Much like physical exercise, laughter raises your heart rate and can lower blood pressure, promoting cardiovascular health. Additionally, it helps calm the body’s stress response by reducing levels of cortisol, the primary stress hormone, leaving you feeling more relaxed and resilient. In fact, a series of six experimental studies found that pain thresholds were significantly higher after laughter compared to conditions without laughter, highlighting its potential as a natural pain-relief strategy.
Ways to Find Humor
- Look up a joke of the day or listen to a funny podcast
- Watch a comedic movie or TV show
- Join fun group activities like karaoke or laughter yoga
- Relive funny memories or share a humorous story with friends

Positive Thinking
Thinking positively is more than just “looking on the bright side”—it’s a powerful tool for healing and pain management. Studies show that optimism can improve overall well-being, reduce stress, and even support the immune system. People who think positively often handle challenges better and recover more quickly from surgery or illness. Optimistic thinking helps shift your focus away from pain and onto the things you can control, making it easier to cope with discomfort and stay motivated throughout recovery.
- Self-Affirmations: Repeat positive statements that reinforce your ability to cope.
- Gratitude Journaling: Write down daily reflections of things you’re thankful for.
- Surround Yourself with Positivity: Spend time with uplifting friends, family, or faith-based communities.
- Focus on Change: Reframe challenges as opportunities for growth and healing.